Many channels and chambers on the surface and inside the human body are covered with a layer of protective barrier called the “mucosa,” acting essentially as an armor for the body, capable of effectively protect the body from threats of foreign pathogens and viruses. Moreover, the mucosa also has multiple functions, including secretion, absorption and perception, making it able to offer the body an all-round protection.
The mucosal organs generally refer to the cavity and mouth, such as: oral mucosa, conjunctiva, nasal mucosa, gastric mucosa, digestive tract mucosa, rectum mucosa, esophagus mucosa, vaginal mucosa…etc. The skin and the mucosa protect the human body, enabling the body to form a closed system to the outside world. When harmful substances are about to invade the body through the oral mucosa, the skin and the mucosa will first block off and keep the external virulence factor away from the body. The mucosal area in an adult human body is approximately 400 square meters, a number that is significantly greater than the 2 square meters of skin. The huge difference in area is a clear indication that foreign pathogens can more easily invade the human body, which is why the mucosa has its own set of defense mechanisms.
There is a wide range of diseases associated with mucosal damage. In fact, various disciplines, such as stomatology, dermatology and venereology, otolaryngology, and internal medicine, all value mucosal completeness as critically important.
Damage to the oral mucosa increases the risk of pathogen entering from the mouth, which causes inflammation and ultimately leads to the imbalance of the immune system.
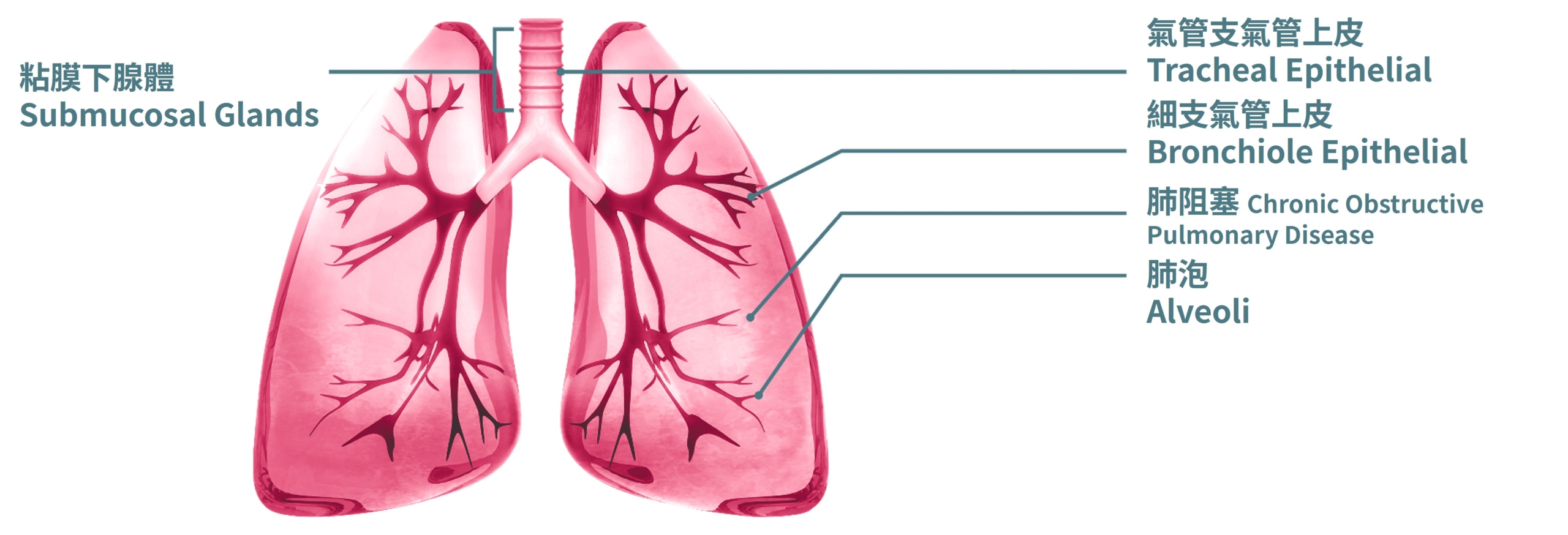
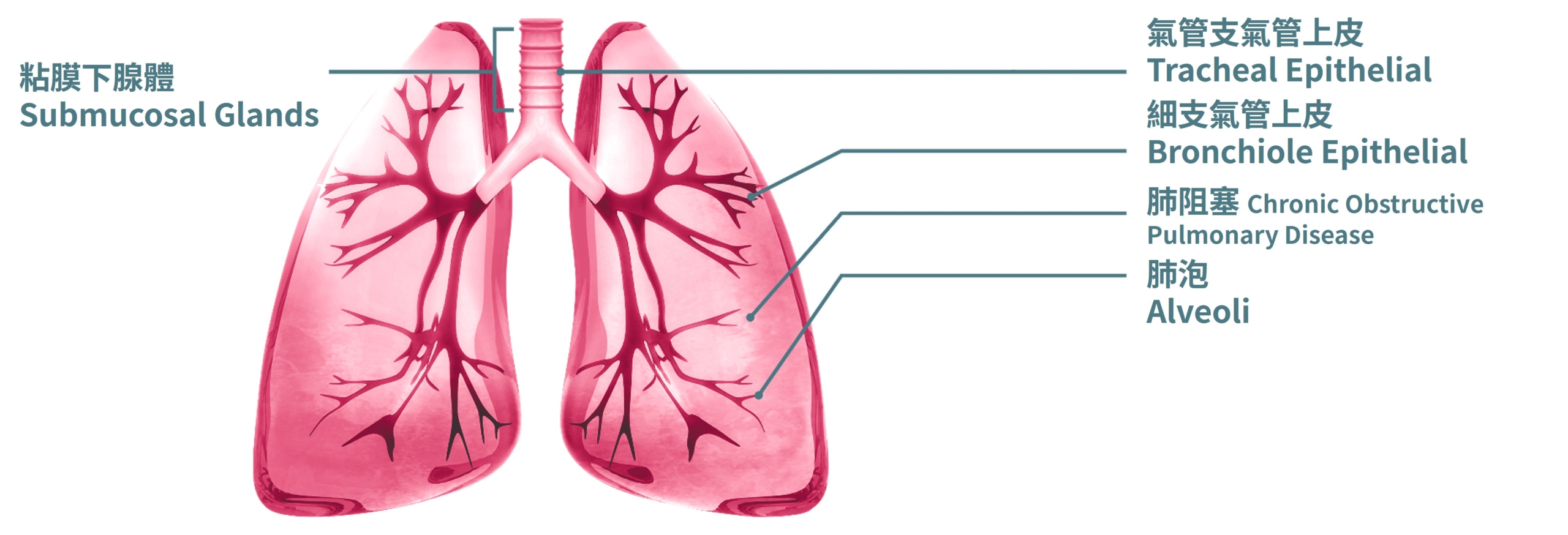
Damage to the mucosa in the respiratory tract increases the chances of infections.
- Destruction to the first-line barrier, enabling viruses and bacteria to enter unhinged, directly causing diseases.
- Resulting from the imbalance of oral microbiome, periodontal bacteria is able to wreak havoc, which causes periodontal disease, gum atrophy, bad breath, and damage to the nerves under the mucosa. In more severe cases, it can cause autoimmune diseases.
- Etiological or physical decrease in saliva can also lead to an increase in friction, which in turn causes damage to the oral mucosa. For example, ole age, chemotherapy, autoimmune diseases.

- A decrease in the functions of the immune system will lead to a decrease in the number of immune cells in the mucosa, and in turn causing a decrease in the number of musical epithelial cells, preventing it from effectively defending against foreign pathogenic bacteria.
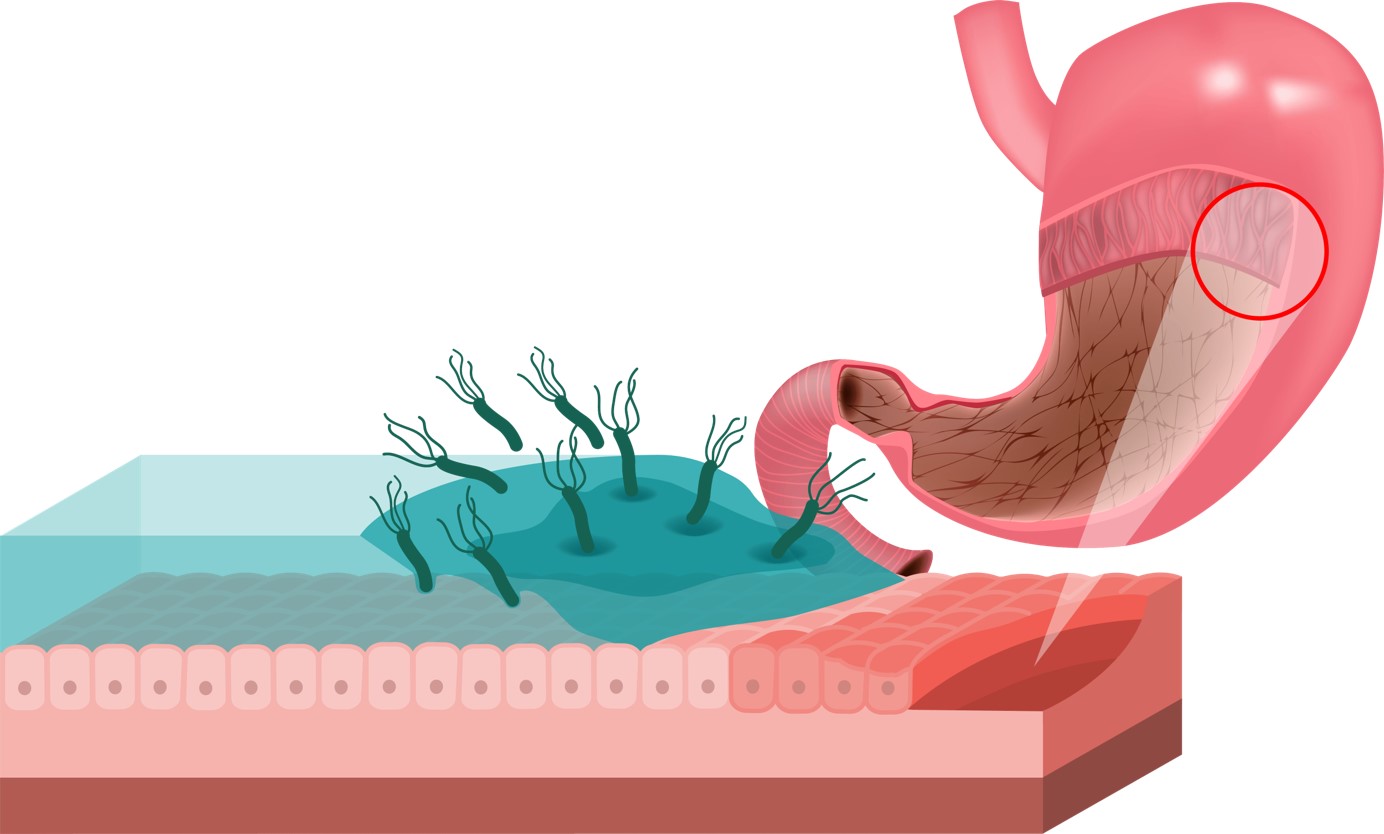
Damage to the gastric mucosa leads to a decrease in quality of life and consumption of food
- The entirety of inner surfaces of the stomach is covered with a layer of mucosal tissue, which is capable of secreting mucus, protecting the gastric tissue by forming a mucus-mucosal barrier in the stomach so that the stomach won’t be affected by gastric acid; Gastric mucosal damage is commonly seen in gastritis or gastric ulcers.
- Previous beliefs have thought that gastric mucosal damage is the result of improper food consumption or bad lifestyle choices, such as smoking, drinking, strong tea, coffee, or medicine that stimulates the gastric mucosa such aspirin, or any other anti-inflammatory drugs. However, with the ever-increasing rapid pace of life living in the society, there is an obvious growing trend in stress-induced ulcers caused by dysbiosis originating from the unwarranted secretion of adrenaline due to excessive stress.
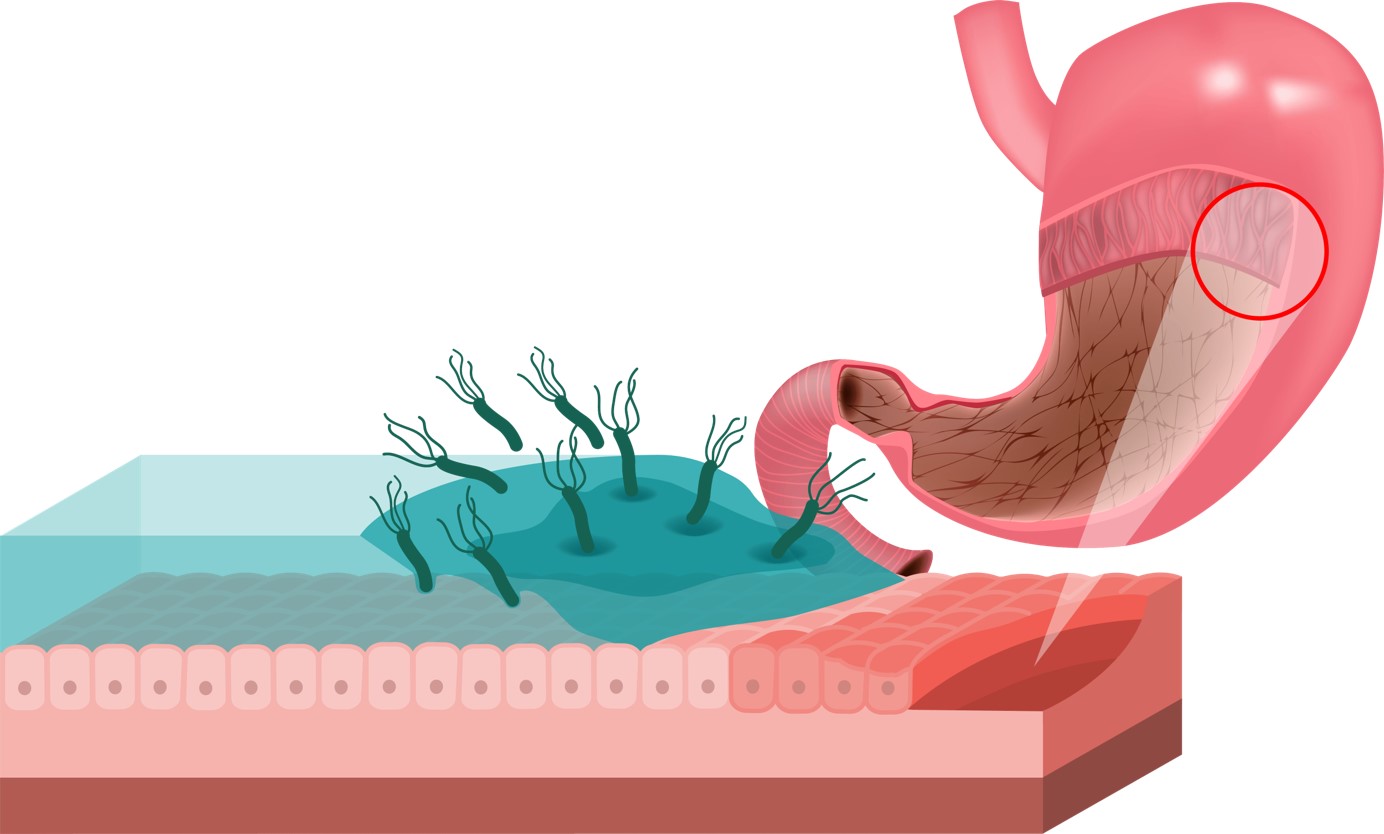
- As damage to the mucosa occurs when inflammation of the stomach is prolonged, the mucosa will begin to shrink and form atrophic gastritis, and could even cause metaplasia in the gastric mucosa, which may ultimately turn into gastric cancer.
- Damage to the gastric mucosa can cause gastric acid to act directly on the stomach wall, which leads to ulcers.
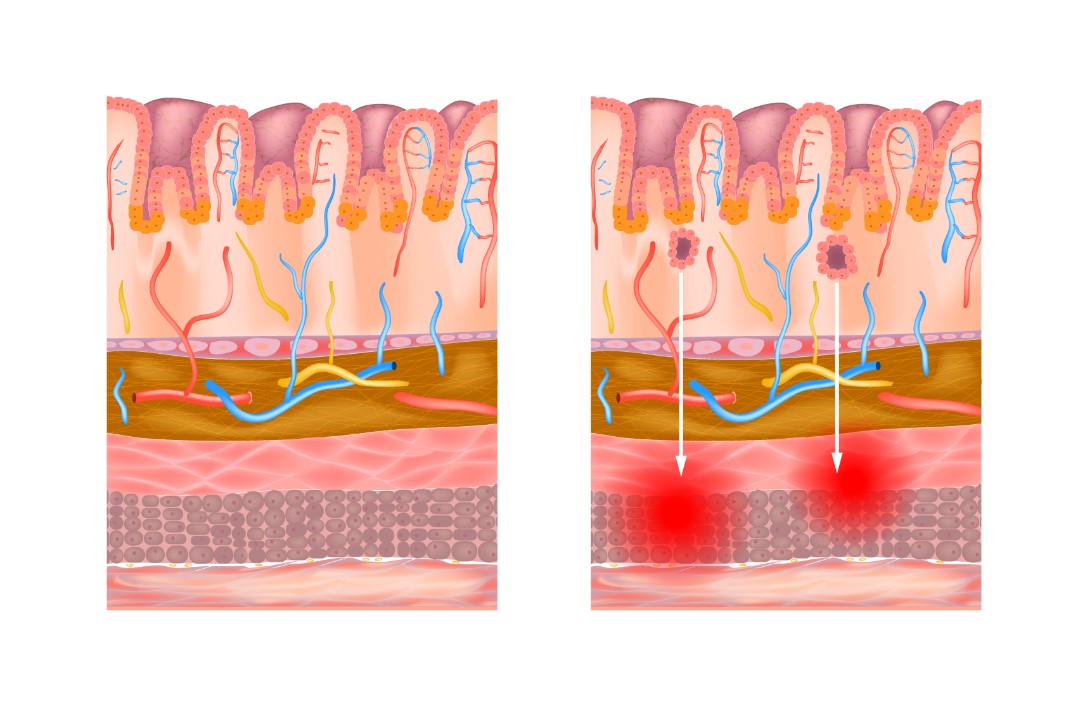
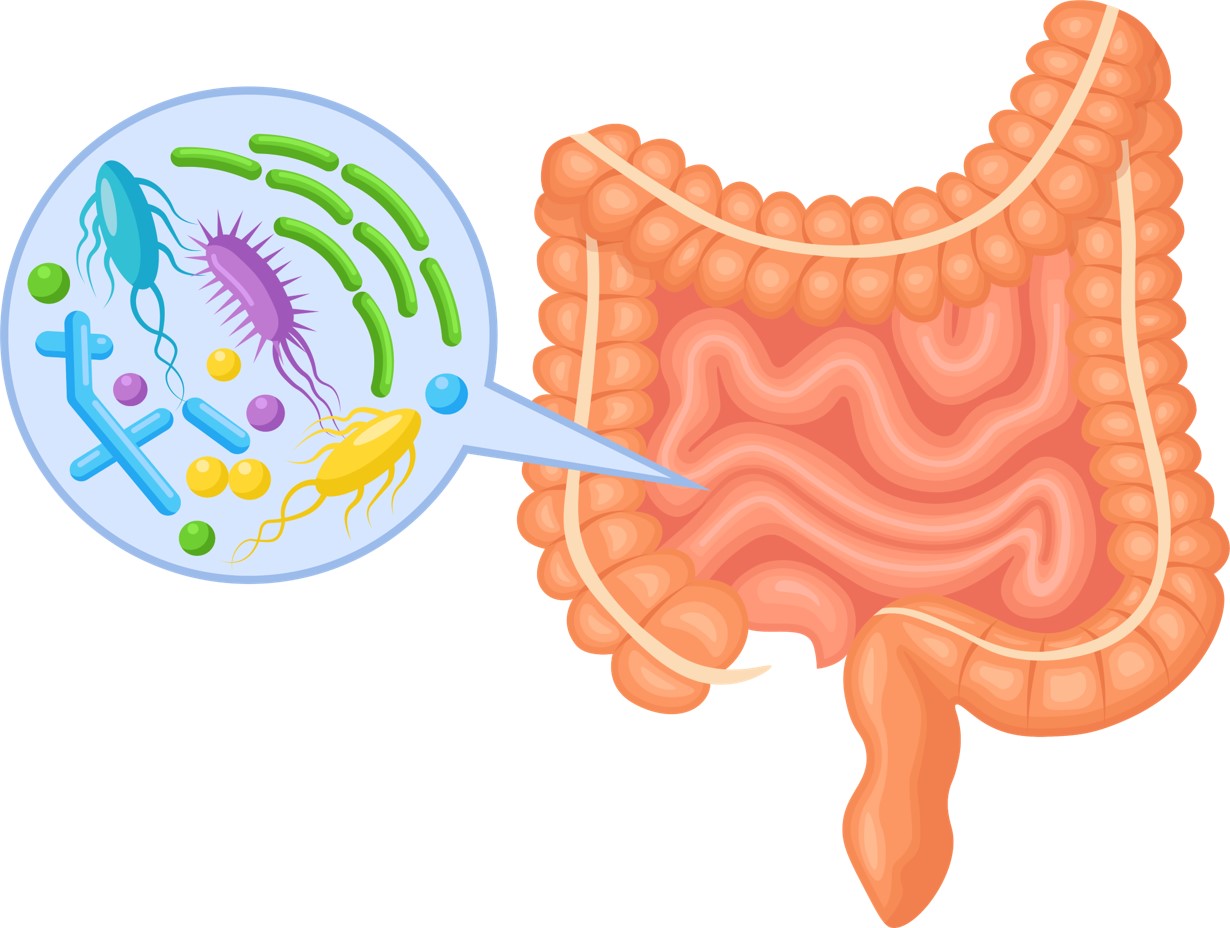
Damage to the intestinal mucosa – Chronic inflammation, Changes in gut microbiota, leaky gut syndrome
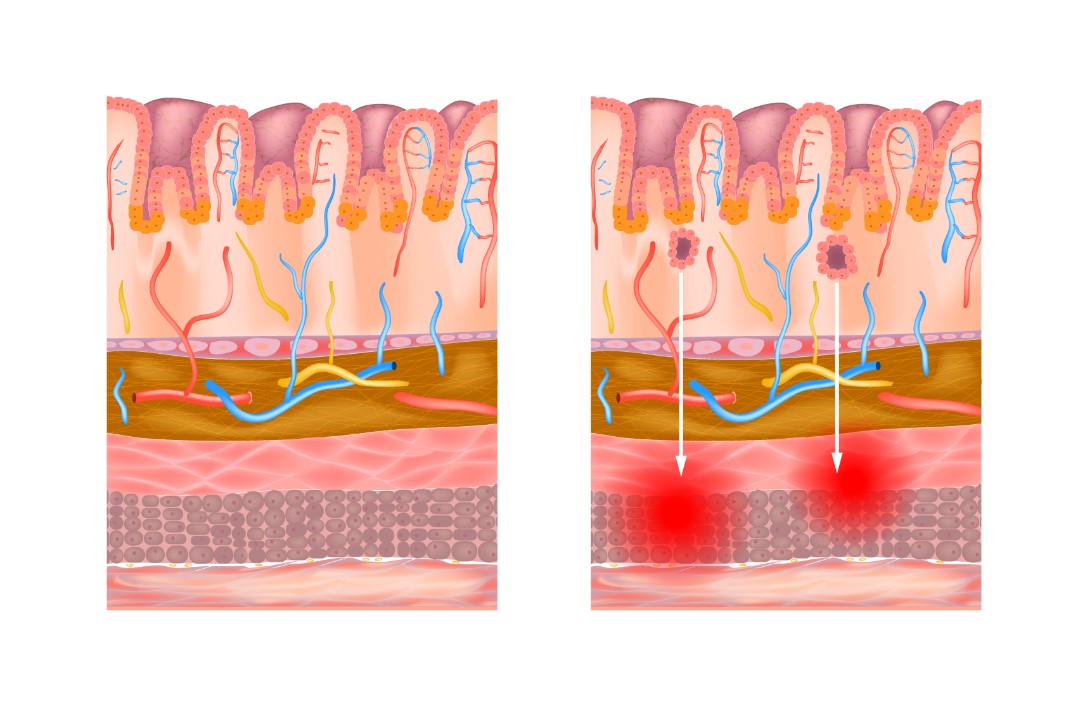
- Maintaining a stable state of gut microbiota can assist in the maintenance of intestinal wall completeness and is beneficial in the preventing the occurrence of leaky gut syndrome. Gut microbiota imbalance can lead to a decrease in the diversity of gut microbiota, causing a reduction in the number of beneficial flora while increasing the number of harmful flora. This then leads to damage and inflammation of the intestinal membrane, ultimately prompting the occurrence of leaky gut syndrome, and in turn causing the imbalance of the immune system of the entire body.
- Damage to the intestinal mucosal cells that result in leak gut syndrome will not only cause inflammatory bowel disease (IBD), it could even let toxins, allergens, pathogens directly enter into the lamina propria of the mucosa, and in turn causing the imbalance and chaos in the immune system.